TESTICULAR CANCER
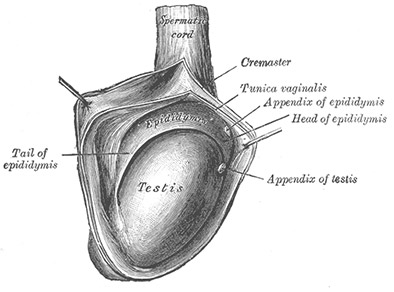
The testicles are two small, egg-shaped glands located close to the penis. The loose skin that surrounds them is called the scrotum. Testicles contain many specialised cells, including germ cells, which make sperm, and other specialised cells that make testosterone.
Testicular cancer is a relatively rare disease. Each year, it affects about 800 men in Australia, many of them between the ages of 18 and 39.
ADDITIONAL INFORMATION
Testicular cancer isn’t linked to any habits, activities or lifestyles. However, there are two important risk factors that can increase your chance of getting the disease.
- An undescended testicle: Testicles drop down from the abdomen to the scrotum before you’re born. If you were born with an undescended testicle, you have a greater risk of testicular cancer, even if you’ve had surgery to fix the issue.
- A previous testicular cancer diagnosis: If you’ve been diagnosed with cancer in one of your testicles, you’re more likely to get cancer in the other one.
TYPES About 95 percent of testicular cancers begin in germ cells, specialised cells in the testicles that make sperm. While these tumours typically start in the testicles they can also occasionally arise in the abdomen, chest, or other areas of the body, even if there’s no evidence of cancer in or near the testicles.
Two of the most common germ cell tumours are seminoma and non-seminoma.
- Seminomas make up about half of all germ cell tumours. They usually grow slowly. Early-stage seminomas can often be cured because they’re less likely to metastasise (spread) to other parts of the body.
- Non-seminomas are often more aggressive than seminomas, and more likely to spread beyond the testicle.
About 5 percent of testicular cancers start in stromal cells, which make testosterone. However, testicular stromal tumors are often benign (not cancerous). A stromal cell tumor could also be a cancer that has spread from another part of the body (called a secondary cancer).
The most common symptoms of testicular cancer are pain, swelling, or a lump or hardness in the testicles. Any testicular lump should be brought to the attention of your doctor immediately.
Less common symptoms include:
- lower abdominal or groin pain
- tenderness in the breast area
- a painless lump in the testicle
- heaviness in the scrotum
- back pain
While these symptoms don’t necessarily mean cancer is present, see a doctor if you experience any of them — early detection greatly increases your chance of successful treatment.
If you have found a lump or swelling in your testicles, your first appointment will include a complete examination of your testicles and abdomen. We will also order blood tests to measure certain tumour markers levels, which may indicate the presence of tumours and help determine your prognosis.
If needed, imaging tests may be ordered, including ultrasounds or CT scans. These tests can help find cancerous tumours and determine if they’ve spread to other parts of your body
If tests indicate that you have a germ cell tumor, we will use the results to help identify how advanced it is and choose the right treatment for you.
The TNM system is used to determine how advanced your tumour is.
- T: the size of your testicular tumour
- N: whether your cancer has spread to the lymph nodes in the pelvis or abdomen
- M: whether your cancer has metastasised (spread) to other parts of the body
We categorise testicular cancer into three stages:
- Stage I, when the cancer is only in the testicle with no evidence that it has spread
- Stage II, when the cancer has spread to nearby lymph nodes in the abdomen or pelvis
- Stage III, when the cancer has spread to lymph nodes in the chest, lungs, liver, bones, or brain
Your doctor may add a letter (A, B, C, or S) to these stages to more precisely describe the cancer.
ADDITIONAL INFORMATION RISK FACTORS TYPES SYMPTOMS OF TESTICULAR CANCER TESTICULAR CANCER DIAGNOSIS STAGES SURGERY Surgery is an important part of diagnosing testicular cancer. In the surgical procedure, which is called a radical orchidectomy, we remove the affected testicle and examine the tumour to identify which type of tumour you have: seminoma, non-seminoma, or something less common. This information helps your doctors choose the right treatment for you.
If diagnostic tests indicate that you have a germ cell tumor, the next step is to assess how advanced the tumour is through a process called staging.
Surgery is usually the primary treatment for early-stage seminomas and non-seminomas that haven’t metastasised (spread). For more aggressive or advanced testicular cancer, you may require referral to a medical oncologist for chemotherapy.
With a procedure called radical orchidectomy, surgeons remove the tumour along with the testicle. This highly effective surgery is usually used early on in diagnosis and staging of testicular cancer. When combined with lifelong monitoring, it may be the only treatment needed for early-stage germ cell tumors that haven’t spread beyond the testicle.
This surgery won’t affect your fertility or your ability to get and keep an erection.
We offer you the option to have a prosthetic testicle inserted during surgery. This is purely a cosmetic choice.
Chemotherapy can eliminate cancer cells throughout the body. Your doctor may recommend this approach if you have testicular cancer that is at a more advanced stage or likely to metastasise (spread). This treatment can also prevent the return of advanced seminomas and non-seminomas that have spread.