VASECTOMY
Vasectomy is an operation designed to produce sterility in a man. It is the most effective form of contraception and over 30 million men worldwide have had the operation.
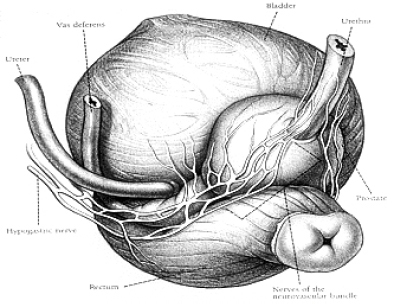
The vas is a muscular tube which conducts sperm from the testicle to the penis prior to ejaculation. It is about 6mm in diameter and can be felt as a taut cord in the scrotum (the best time to do this is in the bath).
During a vasectomy a piece of the tube between 1cm & 2cm long is removed from both the right and left sides. This interrupts the flow of sperm, and after a period of time no sperm are found in the semen. The patient is then sterile.
ADDITIONAL INFORMATION
The operation can be performed using a local anaesthetic injection with the patient awake, or using a general anaesthetic during which a patient is asleep. Either method of anaesthesia is acceptable but patients who are nervous often prefer to have a general anaesthetic so that they feel nothing during the surgery. If local anaesthetic is used the patient may feel some pulling on the testicle which is said to feel rather like having had a kick in the testicles. Two stitches are used to close the wound and usually these will be self-dissolving stitches. The operation is always done as a day case.
Any operation carries risks and vasectomy is no different. The risks are small. If a general anaesthetic is chosen there is a minute risk of anaesthetic related death estimated to be about 1 in 100,000. The main complication close to the time of the operation is bleeding. About 1% of patients develop a haematoma or large bruise in the scrotum, which can make the scrotum swell rather alarmingly, sometimes to the size of a grapefruit. This is rare but not surprisingly causes pain and distress. If a large haematoma develops a second procedure may be required to evacuate the blood clot, and the swelling will take several weeks to resolve. Most patients (99%) do not develop large amounts of bruising and in them the pain and swelling usually resolved in a week or so, and is controlled easily by taking paracetamol.
In the longer term the main hazard is the development of testicular aching or pain. The incidence of this complication is difficult to estimate but may be as high as 1%. The pain can be quite distressing and all urologists see patients in their clinics every year who are very unhappy when this sort of pain develops. This is rare but may be more common in people who already have a discomfort within the testicle for whatever reason. Its cause is unclear but may because of engorgement and stretching of the epididymis and testicle by sperm that continue to be produced by the testicle but have nowhere to go. A second cause of pain in the long term is the development of a tender lump at the site of division of the vas. This is probably due to leakage of sperm from the cut end of the vas and the reaction of the body’s immune system to these sperm that produces inflammation and pain.
There is no good evidence that having a vasectomy is associated with the development of tumours in the future. Many studies have been performed exploring a possible link between vasectomy and prostate cancer and testis cancer but the link is unproven.
A patient is not sterile immediately following a vasectomy as it can take three to six months for the sperm to clear from the ejaculate. The more times a patient ejaculates in the three months following the procedure the more likely it is they will be clear on checking we recommend 25 ejaculates prior to the first check. Patients are advised to produce two semen samples, one week apart, approximately three months post-surgery, and if these show no sperm in them then the patient can be considered sterile, and can discontinue contraceptive measures. If the samples are not clear, they are repeated monthly until they are clear.
Many patients wonder if sexual performance will be altered by vasectomy it is not. The ability to achieve an erection and ejaculate is unchanged. The volume of the ejaculate is also unchanged, as most of the ejaculate comes from the seminal vesicles not the testicles. The seminal vesicles are unaffected by vasectomy.
Although vasectomy is reliable as a method of contraception it is not foolproof. In a small number of individuals the tubes may rejoin spontaneously and sperm may reappear in the ejaculate. This eventuality is rare and the risk of fathering another child is around 1 in 3000.
Doctors and patients differ in their answers to this difficult question. A man who is uncertain about whether or not he wants further children should not have a vasectomy as the operation can to all intents and purposes, be considered irreversible.
Many surgeons are reluctant to offer the operation to young men, say less than 30 years of age. This is because many men who get divorced and later remarry may wish to have children with their new wife. This is difficult if they have already had a vasectomy.
Patients who already have pain in the testicles prior to a vasectomy are probably best advised to avoid vasectomy as their method of contraception. A testicle that is already sore or sensitive may be made more sensitive once the vasal tubes are severed.
If a man has had a vasectomy and changes his mind at a later date about the desirability of further children, an operation can be performed to rejoin the severed tubes a vasectomy reversal. The aim is to restore continuity to the tubes and allow sperm to flow into the ejaculate again.
A vasectomy reversal is a much more complex procedure than a vasectomy and is always performed under general anaesthesia. The operation takes about two hours and is technically demanding. The ends are usually rejoined under magnification and some surgeons use an operating microscope to allow the accurate placement of the very fine stitches.
The success of the operation depends on the skill of the surgeon and the length of time that has elapsed since the vasectomy. If the reversal takes place within three years of the vasectomy then sperm will usually be found in the ejaculate after the reversal, and 75% of couples will achieve a pregnancy. If between three and eight years have elapsed around 50% of couples achieve a pregnancy. Only around a third of couples will achieve a pregnancy if more than 10 years has elapsed since the vasectomy.
If the operation fails, a pregnancy can still sometimes be achieved using techniques of in vitro fertilisation (IVF) using sperm harvested from the epididymis, testis or vas. Sperm can be collected for deep frozen storage at the time of the reversal operation so that if the reversal operation is unsuccessful, the frozen sperm can be used for IVF. This means that the patient does not have to undergo a separate operation at some point in the future to have sperm harvested.